Sunscreens are important photo-protective measures.
These are available in different SPF factors.
Higher the SPF the higher sun protection achieved.
SPF is sun protection factor.
It is a measure to assess protection against UVB radiations.
SPF= minimal erythema induced after exposure of sun protected skin
----------------------------------------------------------------------------
Minimal erythema induced after exposure of unprotected skin
UVA protection is also important for complete sun protection.
UVA protection is assessed on the basis of persistent pigment darkening (PPD).
It's called UVA -PF ( Ultraviolet A - protection factor).
Two different types of sunscreen :
Chemical and physical sunscreen
(Organic and inorganic)
Avobenzone is most commonly used UVA filter.
Octinoxate is widely used UVB filter.
Inorganic active ingredients :
Titanium dioxide and zinc oxide
These particles available in microfine particles ( nano particles) to avoid refraction of light.
Sunscreen should be applied 2 mg/cm2 to achieve accurate sun protection as labeled on sunscreen with SPF.
Controversies:
1) vitamin D:
With sunscreen application serum vitamin D levels which require sunlight will decrease or not??
The answer is No.
Most of the times people apply sunscreen inadequately so not affecting natural process of conversion of cholecalciferol ( vit D3).
The same UVB radiation is required for vit D synthesis so it's not acceptable to get exposed it to induce photocarcinogenesis.
Instead one can take vit D supplements and must continue photo protection with sunscreen .
2) melanoma and nonmelanoma skin cancer
Is sunscreen usage really helpful in reducing skin cancer on prolonged use??
Answer is yes.
Few scientific studies have established the effectiveness of sunscreen in decreased risk of development of skin cancer.
How often one should apply sunscreen ?
Every 2 hours sunscreen should be reapplied.
As sunscreen do migrate to skin surface through follicular orifice and lead to uneven distribution.
These can be removed with sweat and water. So reapplication is necessary to remain protected all time.
USAN : United States adopted nomenclature is used to name active ingredient of sunscreen .
Till date 16 active ingredients are included in list by FDA.
New generation sunscreen ingredients are more photo-stable one.
Photo allergy risks with active ingredients are relatively low.
Hi there, I am Dr. Snehal Thorat specialized in Dermatology and cosmetology. Presently taking advance training in lasers at China Medical University Hospital of Taiwan. If you have any skin related issues or about cosmetic problems, please contact me.
Sunday, October 9, 2016
Friday, September 30, 2016
Kimura disease
Kimura disease :
It's one of the rare condition ..
It is characterized by asymptomatic subcutaneous mass which enlarges gradually. Sometimes pruritus or ulcers may be accompanying symptoms.
Sites: head and neck region most commonly affected.
Others: trunk or extremities and sometimes inguinal or epitrochlear lymph nodes.
Superficial glands may be affected: parotid or submandibular gland
It's mostly solitary or can be multiple in number.
IgE and eosinophils are increased in such patients.
Renal system is affected with nephrotic syndrome presentation..
Differential diagnosis :
Lipoma
Subcutaneous tumor
Angiolymphoid hyperplasia with eosinophilia
Histopathology:
Cellular : increased eosinophils and follicular hyperplasia
Vascular : arborizing vascular proliferation of post capillary venules
Fibrocollagenous
Treatment :
Radical excision is first line therapy
Radiotherapy is second line
If multiple masses chemotherapy is preferred
If renal involvement steroids is the first choice.
Recurrence is possible at primary site or other sites.
It's one of the rare condition ..
It is characterized by asymptomatic subcutaneous mass which enlarges gradually. Sometimes pruritus or ulcers may be accompanying symptoms.
Sites: head and neck region most commonly affected.
Others: trunk or extremities and sometimes inguinal or epitrochlear lymph nodes.
Superficial glands may be affected: parotid or submandibular gland
It's mostly solitary or can be multiple in number.
IgE and eosinophils are increased in such patients.
Renal system is affected with nephrotic syndrome presentation..
Differential diagnosis :
Lipoma
Subcutaneous tumor
Angiolymphoid hyperplasia with eosinophilia
Histopathology:
Cellular : increased eosinophils and follicular hyperplasia
Vascular : arborizing vascular proliferation of post capillary venules
Fibrocollagenous
Treatment :
Radical excision is first line therapy
Radiotherapy is second line
If multiple masses chemotherapy is preferred
If renal involvement steroids is the first choice.
Recurrence is possible at primary site or other sites.
 |
| Parotid swelling with subcutaneous swelling on arm |
Tuesday, September 27, 2016
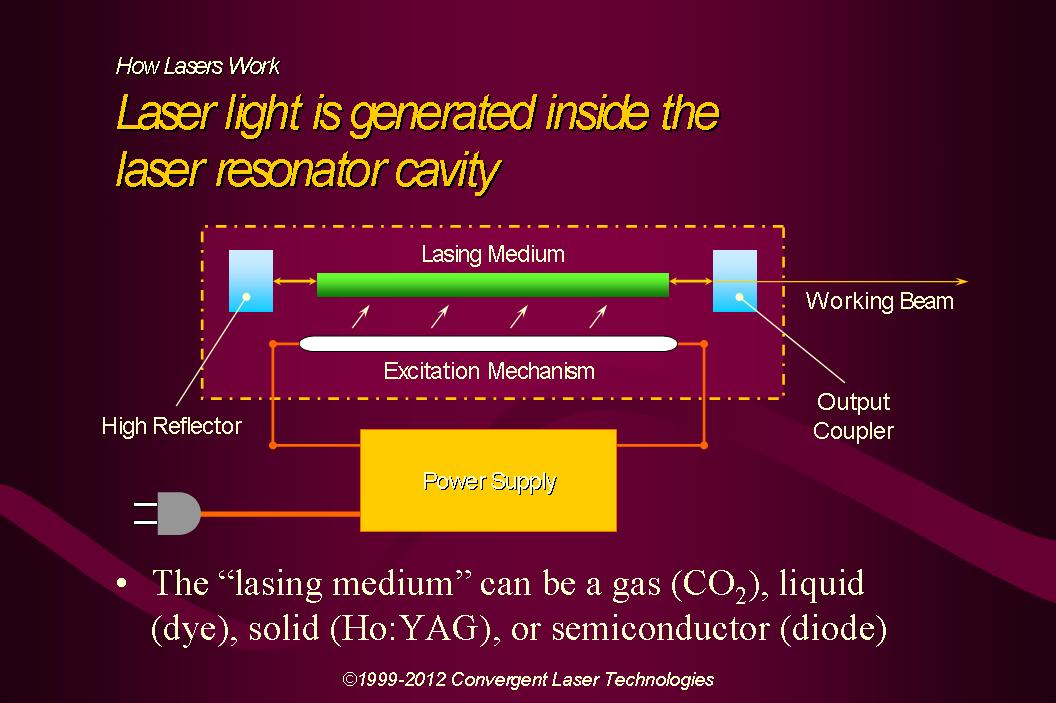
Laser principles
Laser and flash lamps in dermatology :
Laser works on principle of selective photothermolysis.
Leon Goldman started laser use in dermatology first time after discovery of lasers.
Flashlamps are intense pulsed light ( IPL) devices..
These lights use cut off filters so as to provide broad range of wavelengths of electromagnetic spectrum .
IPL can be available for versatile use in dermatology ..
Lasers are collimated monochromatic light energy delivered at specific wavelength with either continuous mode or pulsed waves with pre- determined pulse duration to destroy specific target.
Photons are the quantum of light energy. When photons are stimulated in excited medium they are capable of generating other photons exponentially. These stimulated emission of photons through the mirror with reflectivity <100% concentrated on lens to form laser beam on fiber.
So the name: LASER: light amplification by stimulated emission of radiation .
Selective photothermolysis :
Laser destroys the target inside skin very specifically without damage to adjacent tissue
Basic parameters of optical radiation:
Energy = power * time
Intensity= power/ area
Fluence = power* time /area
Radiant exposure for IPL is determined by size of applicator and energy of radiation.
Energy is expressed in terms of joules.
Fluence is expressed in J/cm2.
Longer the wavelength between 400-1200 nm the more deeper the penetration in the skin.
Lasers are classified as
1)Continuous wave (>0.2 s)
2) pulsed mode (0.2 s-1 micro second)
3) quality switch lasers ( 1 micro second - 1 ns)
Interaction of radiation with skin:
When radiation penetrate the skin the following process can happen:
1) scattering
2) reflection
3) absorption
So when we decide the laser wavelength we should take these optic physics into consideration.
Eye safety is must because of reflection of light.
UVR and Infrared light can not be visible to eye so more chance of damage without perception.
Possible eye injuries range from cornea damage, retina injury, cataracts to permanent blindness.

Laser works on principle of selective photothermolysis.
Leon Goldman started laser use in dermatology first time after discovery of lasers.
Flashlamps are intense pulsed light ( IPL) devices..
These lights use cut off filters so as to provide broad range of wavelengths of electromagnetic spectrum .
IPL can be available for versatile use in dermatology ..
Lasers are collimated monochromatic light energy delivered at specific wavelength with either continuous mode or pulsed waves with pre- determined pulse duration to destroy specific target.
Photons are the quantum of light energy. When photons are stimulated in excited medium they are capable of generating other photons exponentially. These stimulated emission of photons through the mirror with reflectivity <100% concentrated on lens to form laser beam on fiber.
So the name: LASER: light amplification by stimulated emission of radiation .
Selective photothermolysis :
Laser destroys the target inside skin very specifically without damage to adjacent tissue
Basic parameters of optical radiation:
Energy = power * time
Intensity= power/ area
Fluence = power* time /area
Radiant exposure for IPL is determined by size of applicator and energy of radiation.
Energy is expressed in terms of joules.
Fluence is expressed in J/cm2.
Longer the wavelength between 400-1200 nm the more deeper the penetration in the skin.
Lasers are classified as
1)Continuous wave (>0.2 s)
2) pulsed mode (0.2 s-1 micro second)
3) quality switch lasers ( 1 micro second - 1 ns)
Interaction of radiation with skin:
When radiation penetrate the skin the following process can happen:
1) scattering
2) reflection
3) absorption
So when we decide the laser wavelength we should take these optic physics into consideration.
Eye safety is must because of reflection of light.
UVR and Infrared light can not be visible to eye so more chance of damage without perception.
Possible eye injuries range from cornea damage, retina injury, cataracts to permanent blindness.
Monday, August 29, 2016
steatocystoma multiplex
Steatocystoma multiplex:
Definition:
It is also called as epidermal poly cystic disease.
There are numerous epithelial lined sebum filled dermal cysts with characteristic sebaceous gland in the cystic wall.
Associated with Alagille syndrome and pachyonychia congenita type 2.
In these cases defect is K17 mutations.
It can be sporadic occurrence or inherited as autosomal dominant.
Clinical presentation:
Skin coloured cysts on trunk, upper arms, scrotum and chest.
No symptoms
Complication: suppurations and sinus formation leading to scarring.
When single cyst is present in sporadic manner it's called steatocystoma simplex.
Pathological findings:
Cyst is lined by stratified squamous epithelium but no granular layer and sebaceous glands are located on cyst wall.
Eosinophilic cuticle on luminal side of this wall with hair and keratin inside it.
Differential diagnosis: eruptive vellus hair cyst
Epidermal inclusion cyst
Treatment:
Surgical excision
Cyst drainage with manual removal of cyst.
Inflamed lesions can be treated with oral retinoids, cryotherapy or CO2 laser or intralesional steroids.
Definition:
It is also called as epidermal poly cystic disease.
There are numerous epithelial lined sebum filled dermal cysts with characteristic sebaceous gland in the cystic wall.
Associated with Alagille syndrome and pachyonychia congenita type 2.
In these cases defect is K17 mutations.
It can be sporadic occurrence or inherited as autosomal dominant.
Clinical presentation:
Skin coloured cysts on trunk, upper arms, scrotum and chest.
No symptoms
Complication: suppurations and sinus formation leading to scarring.
When single cyst is present in sporadic manner it's called steatocystoma simplex.
Pathological findings:
Cyst is lined by stratified squamous epithelium but no granular layer and sebaceous glands are located on cyst wall.
Eosinophilic cuticle on luminal side of this wall with hair and keratin inside it.
Differential diagnosis: eruptive vellus hair cyst
Epidermal inclusion cyst
Treatment:
Surgical excision
Cyst drainage with manual removal of cyst.
Inflamed lesions can be treated with oral retinoids, cryotherapy or CO2 laser or intralesional steroids.
Monday, August 15, 2016
Lasers
Therapeutic applications of lasers:
1. Tattoo removal
2. Vascular lesions:
A. Telangiectasia
B. Port wine stain
C. Infantile haemangioma
E. Venous lake
F. Starburst veins
G. Varicose veins
H. Lymphangioma circumscripta
I. Tuberous sclerosis ( angiofibromas)
3. Tumors:
A. Trichoepithelioma
B. Neurofibromas
C. digital mucous cyst
D. Xanthelesma
E. Syringomas.
 4. Nevi:
4. Nevi:
A. Epidermal nevus
B. Sebaceous nevi
C. Congenital melanocytic nevus
D. Nevus of Ota
E. Nevus zygomaticus
F. Nevus pigmentosus
5. Hair removal
6. Alopecia areata
7. Vitiligo
8. Keloid and hypertrophic scars
9. Acne and acne scars
10. Seborrhoeic keratoses
11. Freckles
12. Solar lentigo
1. Tattoo removal
2. Vascular lesions:
A. Telangiectasia
B. Port wine stain
C. Infantile haemangioma
E. Venous lake
F. Starburst veins
G. Varicose veins
H. Lymphangioma circumscripta
I. Tuberous sclerosis ( angiofibromas)
3. Tumors:
A. Trichoepithelioma
B. Neurofibromas
C. digital mucous cyst
D. Xanthelesma
E. Syringomas.
 4. Nevi:
4. Nevi:A. Epidermal nevus
B. Sebaceous nevi
C. Congenital melanocytic nevus
D. Nevus of Ota
E. Nevus zygomaticus
F. Nevus pigmentosus
5. Hair removal
6. Alopecia areata
7. Vitiligo
8. Keloid and hypertrophic scars
9. Acne and acne scars
10. Seborrhoeic keratoses
11. Freckles
12. Solar lentigo
13. Skin resurfacing
Monday, August 8, 2016
Biological therapy in dermatology
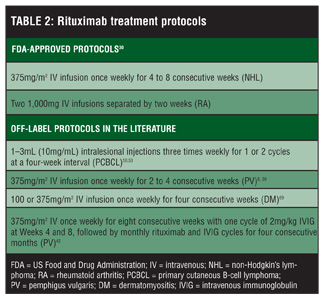
Rituximab 375mg/m2 weekly for 4weeks in pemphigus
Mechanism of action for Rituximab:
It is anti CD20 monoclonal antibody.
Biological agents in psoriasis:
1) Ustekinumab:
45 mg SC on week 0,4, then every 12 weeks
2) Secukinumab:Initial: 300 mg SC at weeks 0, 1, 2, 3, and 4
Monthly maintenance: Beginning at week 8, give 300 mg SC once monthly
For some patients, a dose of 150 mg may be acceptable
3) Adalimumab: 80mg SC on day 1
40mg on day 8
40 mg every 2 weeks
These agents can be combined with phototherapy or methotrexate.
Mechanism of action for Rituximab:
It is anti CD20 monoclonal antibody.
1) Ustekinumab:
45 mg SC on week 0,4, then every 12 weeks
2) Secukinumab:Initial: 300 mg SC at weeks 0, 1, 2, 3, and 4
Monthly maintenance: Beginning at week 8, give 300 mg SC once monthly
For some patients, a dose of 150 mg may be acceptable
3) Adalimumab: 80mg SC on day 1
40mg on day 8
40 mg every 2 weeks
These agents can be combined with phototherapy or methotrexate.
Ustekinumab has shown maximum disease free period after treatment.
Remember:
All biological agents are found to be less effective in obese patients when used as a monotherapy.
Adalimumab can be used in hidradenitis suppurativa cases.
First generation biological agents for psoriasis: etarncept, Adalimumab, inflixiamb
These agents target TNF -alpha.
Second generation: Ustekinumab acts against IL-12/23( pro- inflammatory cytokines)
Third generation: targets IL-17.
Remember:
All biological agents are found to be less effective in obese patients when used as a monotherapy.
Adalimumab can be used in hidradenitis suppurativa cases.
First generation biological agents for psoriasis: etarncept, Adalimumab, inflixiamb
These agents target TNF -alpha.
Second generation: Ustekinumab acts against IL-12/23( pro- inflammatory cytokines)
Third generation: targets IL-17.
Tuesday, August 2, 2016
Seborrheic keratoses
Seborrheic keratoses (SK) :
It's a benign epidermal tumour.
It is commonly present in old age.
It's types:
1) Common seborrheic keratoses
2) Skin tags
3) Irritant SK
4) Pigmented SK
5) SK with squamous atypia
6) Stucco keratoses
7) Leser trelat sign
8) Reticulated SK
9) Dermatosis papulosa Nigra (DPN)
10) Clonal SK
Histopathology:
Acanthosis, papillomatosis, pseudo cyst formation, hyper keratosis.
Clinical features:
Stuck on appearance of lesion
Treatment:
Cryotherapy
Electric desiccation
Laser
Surgical excision
Topical flurouracil
Biopsy is recommended when
Rapid growth of lesion
Atypical clinical appearance
Symptomatology
Unusual lesion location
In the above features there is risk of malignant transformation.
Irritant SK may develop in patients who are on chemotherapy especially cytarabine drug.
Lesar Trelat sign:
Eruption of SK on trunk in Christmas tree pattern
Cause: underlying adenocarcinoma of stomach most commonly
Other: adenocarcinoma of lung and colon.
DPN :
Present in skin type 4 and above.
It's a benign epidermal tumour.
It is commonly present in old age.
It's types:
1) Common seborrheic keratoses
2) Skin tags
3) Irritant SK
4) Pigmented SK
5) SK with squamous atypia
6) Stucco keratoses
7) Leser trelat sign
8) Reticulated SK
9) Dermatosis papulosa Nigra (DPN)
10) Clonal SK
Histopathology:
Acanthosis, papillomatosis, pseudo cyst formation, hyper keratosis.
Clinical features:
Stuck on appearance of lesion
Treatment:
Cryotherapy
Electric desiccation
Laser
Surgical excision
Topical flurouracil
Biopsy is recommended when
Rapid growth of lesion
Atypical clinical appearance
Symptomatology
Unusual lesion location
In the above features there is risk of malignant transformation.
Irritant SK may develop in patients who are on chemotherapy especially cytarabine drug.
Lesar Trelat sign:
Eruption of SK on trunk in Christmas tree pattern
Cause: underlying adenocarcinoma of stomach most commonly
Other: adenocarcinoma of lung and colon.
DPN :
Present in skin type 4 and above.
Tattoo removal
Tattoo removal:
Tattoos are developed with different colours.
Tattoo made by India ink or graphite are easy to remove.
But tattoos made by green,yellow and orange inks are resistant to laser treatment.
Black tattoos show good response to laser therapy.
Methods to remove tattoo:
1) Deep cryotherapy
2) CO2 laser vaporisation
3) Salabrasion
4) Dermabrasion
5) Topical agents
These methods can cause scarring as side effect.
Lasers are good option but recurrence or incomplete removal do happen.
Mechanics behind laser:
Pigment in dermal phagocytes is exposed to temp upto 300 degrees in nanoseconds. This leads to rupture of cell and alteration of chemicals.
Remember:
Red tattoo should be treated by green laser (Q-switched Nd YAG) 532 nm
Green tattoo must be cleared by red colour laser ( ruby 694 nm) or alexandrite laser.
Different colours need to be treated with appropriate corresponding wavelengths of laser.
Multiple sessions of laser are required.
Immediate side effect:
1) Immediate whitening of skin over tattoo is end point of laser therapy.
This will disappear few minutes after cessation of laser treatment as gas bubbles of laser settle down.
2) Epidermal pigment cells also suffer in laser treatment so transient hypo pigmentation occurs.
The risk of scarring from Q- switched laser treatments is approximately 5 percent.
Tattoos are developed with different colours.
Tattoo made by India ink or graphite are easy to remove.
But tattoos made by green,yellow and orange inks are resistant to laser treatment.
Black tattoos show good response to laser therapy.
Methods to remove tattoo:
1) Deep cryotherapy
2) CO2 laser vaporisation
3) Salabrasion
4) Dermabrasion
5) Topical agents
These methods can cause scarring as side effect.
Lasers are good option but recurrence or incomplete removal do happen.
Mechanics behind laser:
Pigment in dermal phagocytes is exposed to temp upto 300 degrees in nanoseconds. This leads to rupture of cell and alteration of chemicals.
Remember:
Red tattoo should be treated by green laser (Q-switched Nd YAG) 532 nm
Green tattoo must be cleared by red colour laser ( ruby 694 nm) or alexandrite laser.
Different colours need to be treated with appropriate corresponding wavelengths of laser.
Multiple sessions of laser are required.
Immediate side effect:
1) Immediate whitening of skin over tattoo is end point of laser therapy.
This will disappear few minutes after cessation of laser treatment as gas bubbles of laser settle down.
2) Epidermal pigment cells also suffer in laser treatment so transient hypo pigmentation occurs.
The risk of scarring from Q- switched laser treatments is approximately 5 percent.
Monday, August 1, 2016
Intolerance to cosmetics
1) Examine every cosmetic and skin-care product
2) Administer patch and photopatch tests to rule out occult
allergic and photoallergic dermatitis
3) Test for contact urticaria
4) Do careful repeat open application testing (ROAT)
5) Treat endogenous inflammatory disease
6) Limit skin-care to:
Water washing without soap or detergent
Lip cosmetics as desired, if lips are clear
Eye cosmetics as desired, if eyelids are asymptomatic
Face powder
Glycerin and rose water as a moisturizer, if necessary.
Cosmetic intolerance syndrome:
It is extreme end of irritant or allergic contact dermatitis to cosmetic products.
Patient can not tolerate any cosmetics over face due to burning sensation.
Definition :
It is an uncommon clinical phenomenon in which patients complain of facial burning and discomfort associated with application of most skin-care products.
Severity of symptoms does not match objective signs of disease.
status cosmeticus: condition in which patients no longer tolerate the use of any facial cosmetic product.
irritation to occult allergic contact dermatitis, allergic photocontact dermatitis, contact urticarial reaction, or a combination can be presenting symptoms.
Investigations:
careful clinical review and patch testing of casual agents.
Advice:
prolonged program of eliminating cosmetics is important.
dermatologic nondisease: facial burning continuously, without showing objective signs.
Saturday, July 30, 2016
Aquagenic syringeal acrokearatoderma
Aquagenic syringeal acrokeratoderma:
It is eccrine gland disease.
Pathogenesis is poorly understood
Stratum corneum dysfunction and aberration in eccrine gland structure can be possible for the disease presentation.
Clinical features:
Patient complains of appearance of whitish translucent Papules over palms after immersion of hand in water.
Once the contact with water is removed it disappears in 10-20 minutes.
Sometimes it is accompanied by sensation of tingling and tightness of palm.
Excessive wrinkling of skin over palms develop on repeated exposures
Other sites:
Dorsal hands or fingers
Rarely sole is involved
Associations:
Cystic fibrosis
Family history (+) in some cases
Hyperhidrosis
Conditions should be distinguished from hereditary papulotranslucent acrokearatoderma.
Histopathology is helpful to confirm diagnosis
On histopathology orthokeratosis and dialated eccrine ducts are seen in aquagenic acrosyringeal kearatoderma while eccrine gland is normal in hereditary variant.
Treatment:
No standard treatment is available
Options:
1) Aluminum chloride hexahydrate 20% at night
2) Barrier emollients petroleum based
3) 12% ammonium lactate cream
4) Botulinum toxin injection
Biopsy should be performed immediately after immersion of hand in water.
This disease is rare but sometimes it may be under diagnosed.
The hand in bucket sign is very typical of this condition.
It is eccrine gland disease.
Pathogenesis is poorly understood
Stratum corneum dysfunction and aberration in eccrine gland structure can be possible for the disease presentation.
Clinical features:
Patient complains of appearance of whitish translucent Papules over palms after immersion of hand in water.
Once the contact with water is removed it disappears in 10-20 minutes.
Sometimes it is accompanied by sensation of tingling and tightness of palm.
Excessive wrinkling of skin over palms develop on repeated exposures
Other sites:
Dorsal hands or fingers
Rarely sole is involved
Associations:
Cystic fibrosis
Family history (+) in some cases
Hyperhidrosis
Conditions should be distinguished from hereditary papulotranslucent acrokearatoderma.
Histopathology is helpful to confirm diagnosis
On histopathology orthokeratosis and dialated eccrine ducts are seen in aquagenic acrosyringeal kearatoderma while eccrine gland is normal in hereditary variant.
Treatment:
No standard treatment is available
Options:
1) Aluminum chloride hexahydrate 20% at night
2) Barrier emollients petroleum based
3) 12% ammonium lactate cream
4) Botulinum toxin injection
Biopsy should be performed immediately after immersion of hand in water.
This disease is rare but sometimes it may be under diagnosed.
The hand in bucket sign is very typical of this condition.
Multiple whitish Papules over palm after water exposure
Thursday, July 28, 2016
Freckles
Freckles:
It is pigmentory condition.
It's also called ephelids.
Freckles are brownish pigmented Macules of various sizes over face.
Other sites: axilla and inguinal regions.
When these sites other than face are involved then we suspect neurofibromatosis type 1.
Freckles are also present in one genodermatoses called xeroderma pigmentosa.
Most patients have freckles only over face. In that case it's very easy to treat it.
Diagnosis is solely based on clinical examination.
Treatment:
1) Topical treatment:
A)Use of Depigmenting agents : Kojic acid
B) Phenol 80% over spots
2) lasers:
a)Frequency doubled Nd. YAG 532 nm
b) IPL (500-1000 nm )
c) Q switched ruby laser 694nm
d) 755nm alexandrite laser
e) 532 nm KTP laser
3)chemical peel
Side effects: post inflammatory hyper or hypo pigmentation.
Remember: freckles don't require treatment always.
When cosmetic concern is there treatment options can be chosen.
Freckles do have 2.5 fold increased risk of sunburn and poor response to tanning.
Difference between freckles and lentigo:
Freckles. Lentigo
1) Darkening on sun exposure No change
2) Presents in early childhood Elderly people
3) No increase in melanocyte Increase in melanocyte number
Number
Use of sunscreen with spf 30+ is strongly recommended in these patients.
It is pigmentory condition.
It's also called ephelids.
Freckles are brownish pigmented Macules of various sizes over face.
Other sites: axilla and inguinal regions.
When these sites other than face are involved then we suspect neurofibromatosis type 1.
Freckles are also present in one genodermatoses called xeroderma pigmentosa.
Most patients have freckles only over face. In that case it's very easy to treat it.
Diagnosis is solely based on clinical examination.
Treatment:
1) Topical treatment:
A)Use of Depigmenting agents : Kojic acid
B) Phenol 80% over spots
2) lasers:
a)Frequency doubled Nd. YAG 532 nm
b) IPL (500-1000 nm )
c) Q switched ruby laser 694nm
d) 755nm alexandrite laser
e) 532 nm KTP laser
3)chemical peel
Side effects: post inflammatory hyper or hypo pigmentation.
Remember: freckles don't require treatment always.
When cosmetic concern is there treatment options can be chosen.
Freckles do have 2.5 fold increased risk of sunburn and poor response to tanning.
Difference between freckles and lentigo:
Freckles. Lentigo
1) Darkening on sun exposure No change
2) Presents in early childhood Elderly people
3) No increase in melanocyte Increase in melanocyte number
Number
Use of sunscreen with spf 30+ is strongly recommended in these patients.
Tuesday, July 26, 2016
Moisturizer
Moisturizer:
It is to maintain moisture of your skin.
It is used very routinely by females.
But do you know which moisturizer is the best for you?
I will educate you about the mechanism behind moisturizer...

Types:
1) occlusive
2) humectant 3) emollient
It is to maintain moisture of your skin.
It is used very routinely by females.
But do you know which moisturizer is the best for you?
I will educate you about the mechanism behind moisturizer...

Types:
1) occlusive
2) humectant 3) emollient
Emollient = occlusive + humectant
occlusive:
Beeswax, soybean oil
Humectants: urea, sugar, sorbitol.
Emollient: lanolin
Beeswax, soybean oil
Humectants: urea, sugar, sorbitol.
Emollient: lanolin
Melasma
Melasma :
It is a pigmentory disorder characterised by brownish Macules over face especially cheeks and forehead.
Types:
1) Epidermal
2) Dermal
3) Mixed
Depending on the level of pigmentation into the skin.
Another classification is based on the location of skin affected
1) Malar
2) Mandibular
3) Centrofacial
Woods light is used to determine the type of melasma.
Cause:
1)Increased estrogen levels in females especially pregnancy
2) prolonged sun exposure
When it happens after or during pregnancy it's called chloasma (pregnancy mask).
How to treat??
1) Topical treatment
2) Systemic
3) Laser or light therapy
4) Chemical peel
1) Topical treatment:
A) Depigmenting agents:
1) Kojic acid
2) Mulberry extract
3) Hydroquinone 4%
B) Retinoids
C) Steroids
Most common topical treatment :
Kligman formula (Triple combination formula):
Hydroquinone+ tretinoin+ fluocinonide
1) Systemic treatment:
a) Capsule vitamin c 200mg 1OD for 2-3 months.
b) Tab tranexamic acid 250-500 mg 1OD
2) Lasers:
Nd Yag laser toning 1064 nm is good for maintenance.
Intense pulsed light therapy is another alternative.
3) Chemical peel:
a) Glycolic acid peel 30%
Peeling procedures have downtime so most of the patients don't prefer.
Mesotherapy with tranexamic acid is also tried in some centres.
Recurrence rate is high with any above treatment.
No standard treatment is available. It is all depends on individual skin type.
Advice :
1) Use of sunscreen with spf 50+ and UVA+++
2) Use of wide brimmed hat in mid-day sun
3) Use of retinoids at night time
It is a pigmentory disorder characterised by brownish Macules over face especially cheeks and forehead.
Types:
1) Epidermal
2) Dermal
3) Mixed
Depending on the level of pigmentation into the skin.
Another classification is based on the location of skin affected
1) Malar
2) Mandibular
3) Centrofacial
Woods light is used to determine the type of melasma.
Cause:
1)Increased estrogen levels in females especially pregnancy
2) prolonged sun exposure
When it happens after or during pregnancy it's called chloasma (pregnancy mask).
How to treat??
1) Topical treatment
2) Systemic
3) Laser or light therapy
4) Chemical peel
1) Topical treatment:
A) Depigmenting agents:
1) Kojic acid
2) Mulberry extract
3) Hydroquinone 4%
B) Retinoids
C) Steroids
Most common topical treatment :
Kligman formula (Triple combination formula):
Hydroquinone+ tretinoin+ fluocinonide
1) Systemic treatment:
a) Capsule vitamin c 200mg 1OD for 2-3 months.
b) Tab tranexamic acid 250-500 mg 1OD
2) Lasers:
Nd Yag laser toning 1064 nm is good for maintenance.
Intense pulsed light therapy is another alternative.
3) Chemical peel:
a) Glycolic acid peel 30%
Peeling procedures have downtime so most of the patients don't prefer.
Mesotherapy with tranexamic acid is also tried in some centres.
Recurrence rate is high with any above treatment.
No standard treatment is available. It is all depends on individual skin type.
Advice :
1) Use of sunscreen with spf 50+ and UVA+++
2) Use of wide brimmed hat in mid-day sun
3) Use of retinoids at night time
Monday, July 25, 2016
Skin types
Skin types :
Main four types:
1) dry vs oily
2) pigmented vs non pigmented
3) sensitive vs irritant
4) wrinkled vs tight
With these basic types individual skin can fall in any of 16 types
skin catogerization is important while treating any skin disease
It is important while choosing over the counter cosmetic products.
So the following table will help you to define your skin type.
Oily sensitive skin is more prone to acne and or rosacea.
Pigmented skin should be protected from excessive sun exposure.
Dry skin is likely to develop eczema.
Fitzpatrick skin typing is universal method
Rosacea
Rosacea:
It is chronic inflammatory disease characterized by erythema and pustules.
Histopathology:
1) Dialated dermal vessels
2) Sebaceous gland hyperplasia
3) Inflammatory cell infiltrate
Age group: 20-50 years ( middle age)
Cause: unknown
Exacerbating factors:
1) Spicy food
2) Angry mood / emotional stress
3) Hot weather
4) Hot shower bath for prolonged time
5) Exposure to sunlight
6) Alcohol
7) Exercise
8) Cosmetics
9) Hot drinks
10) Medications
Disease Association with acne is common.
Clinical features:
Sites affected: cheek, nose,forehead,chin
Earliest symptom: flushing
1)Redness over face :
Diffuse erythema over cheeks and nose
Sometimes accompanied by itching and burning sensation
2) prominent telangiectasia
3) Papule and pustules formation
4) sebaceous gland hyperplasia resulting in swelling.
Types of Rosacea:
1) Erythematotelangiectatic (ET)
2) Papulopustular Rosacea
3) Rosacea fulminans ((pyoderma faciale)
4) Rhinophyma ( nose deformity)



Approach to patient:
History of exacerbating factor
Clinical examination with dermatoscope:
For visualization of tiny capillaries
Treatment:
1) Topical treatment
2) Systemic treatment
3) Lasers
It is chronic inflammatory disease characterized by erythema and pustules.
Histopathology:
1) Dialated dermal vessels
2) Sebaceous gland hyperplasia
3) Inflammatory cell infiltrate
Age group: 20-50 years ( middle age)
Cause: unknown
Exacerbating factors:
1) Spicy food
2) Angry mood / emotional stress
3) Hot weather
4) Hot shower bath for prolonged time
5) Exposure to sunlight
6) Alcohol
7) Exercise
8) Cosmetics
9) Hot drinks
10) Medications
Disease Association with acne is common.
Clinical features:
Sites affected: cheek, nose,forehead,chin
Earliest symptom: flushing
1)Redness over face :
Diffuse erythema over cheeks and nose
Sometimes accompanied by itching and burning sensation
2) prominent telangiectasia
3) Papule and pustules formation
4) sebaceous gland hyperplasia resulting in swelling.
Types of Rosacea:
1) Erythematotelangiectatic (ET)
2) Papulopustular Rosacea
3) Rosacea fulminans ((pyoderma faciale)
4) Rhinophyma ( nose deformity)
Approach to patient:
History of exacerbating factor
Clinical examination with dermatoscope:
For visualization of tiny capillaries
Treatment:
1) Topical treatment
2) Systemic treatment
3) Lasers
Sunday, July 24, 2016
Acne vulgaris
Common age: adolescent age 12-25 years.
But it can affect newborns and old aged patients.
Cause: hormone imbalance is the main cause for development of acne
Types:
1] comedones : white heads or black heads
(mild variety)
2] papulopustular acne are of moderate variety
3] nodulocystic acne is severe form of acne
4] acne fulminans and
5]pyoderma faciale
last two forms of acne which require aggressive treatment.


How is this treated?
1] Topical treatments:
Tretinoin 0.025% cream at bedtime is effective in most of patients.
Others: adapalene gel 0.1%, brevoxyl cream, niacinamide gel, clindamycin cream, glycolic acid cream
These creams are useful for mild to moderate acne.
2] systemic/ oral treatments:
Tab azithromycin 500mg once a day for 3 days in a week for 1-3 months
Tab doxycycline 100 mg once daily for 1-3 months.
Tab minocycline 50mg once daily
Tab isotretinoin 0.5-1 mg/kg once daily for 1-6 months
(Isotretinoin treatment is very effective in reducing acne eruption but careful monitoring of liver function and lipid profile is advised). One more important note: Isotretinoin is contraindicated in pregnancy.
Nodulocystic acne can be treated with intralesional triamcinolone acetonide 10 mg/ml.
Treatment of acne fulminans:
Systemic steroids at the beginning to control inflammation and then start antibiotics or isotretinoin.
Systemic steroids at the beginning to control inflammation and then start antibiotics or isotretinoin.
Subscribe to:
Posts (Atom)